The Sunshine Secret: Why Vitamin D Matters for Muscles☀️💪
Jennifer Kummrow2025-06-27T16:34:27+00:00It’s not uncommon to start paying attention to vitamins and supplements when we’re in pain, injured, or sick, but proactive care can support better outcomes before you reach that point! While low vitamin D levels does not equal poor muscle health, maintaining healthy levels can be an important part of the formula for not only sports nutrition, but also healthy aging!
When it comes to bone health and sports injury, we hear a lot about calcium, but the real star might be vitamin D, which also contributes to muscle strength, injury recovery, and immunity. From athletes rehabbing an injury or overtraining, to aging adults striving for a healthy lifestyle – Vitamin D could be a missing link in your rehab and performance journey.
💪 Vitamin D and Muscle Function

Your muscles perform their best when they’re properly supported at the cellular level. While low Vitamin D doesn’t mean poor muscle health, it can quietly set the stage for reduced muscle efficiency. Vitamin D supports your muscles by:
- Supporting muscle contraction by aiding calcium transport and increasing calcium-binding sites in muscle tissue.
- Preserving muscle mass with aging to help reduce the risk of falls.
- Boosting muscle performance such as grip strength, speed, and power.
- Improving VO₂ max, a marker of cardiovascular and muscular endurance.
🦴 Injury Recovery: More Than Rest and Rehab
Vitamin D works alongside calcium to support bone remodeling and repair, which is vital in healing stress fractures and breaks. When vitamin D levels are in the optimal range, people often experience:
- Faster healing from injuries like muscle tears, stress fractures, and tendon strain.
- Less inflammation, which promotes a smoother recovery process.
- Better pain management, thanks to vitamin D’s anti-inflammatory and antioxidant properties.
🛡️ Immunity, Overtraining, and Inflammation
Physical stress—whether from injury, surgery, or intense training—can take a toll on your immune system. Low vitamin D levels have been linked to:
- Higher inflammation
- Weakened Immunity
- Greater fatigue and delayed recovery
Vitamin D helps regulate your immune response and reduces the inflammatory state that often accompanies overtraining or injury. It won’t replace sleep, hydration, or good nutrition—but it plays a vital supporting role.
⚠️ Don’t Just Pop a Pill: Get Tested First
After reading through this information, you may be tempted to just add in a vitamin D supplement, but too much can be harmful! Talk to your doctor and get your levels tested to understand whether supplementing with Vitamin D is right for you.
Common symptoms of Vitamin D deficiency:
- Fatigue
- Muscle and bone pain
- Muscle weakness or cramps
- Mood changes
Common causes of Vitamin D deficiency:
- Not getting enough vitamin D in your diet
- Not getting enough sunlight
- Your body isn’t absorbing vitamin D properly
- High physical stress or chronic pain
Where Can You Get Vitamin D?
- Sunlight (requirements different for everyone depending on skins tone and location)
- Foods (salmon, egg yolks, fortified dairy products)
- Supplement recommended by your healthcare provider
✅ Final Thoughts
Vitamin D isn’t a magic fix, but it is an important part of the puzzle! Whether your goal is strength, healing or resilience, it’s worth checking your vitamin D levels as an important part of your overall recovery and wellness.
 Being ‘healthy’ is more than just avoiding illness or eating fruits and veggies every day. It’s about maintaining balance in your physical, mental and social well-being. While you may begin physical therapy with the goal of reducing pain or healing an injury, PT can also provide significant benefits for your mental health.
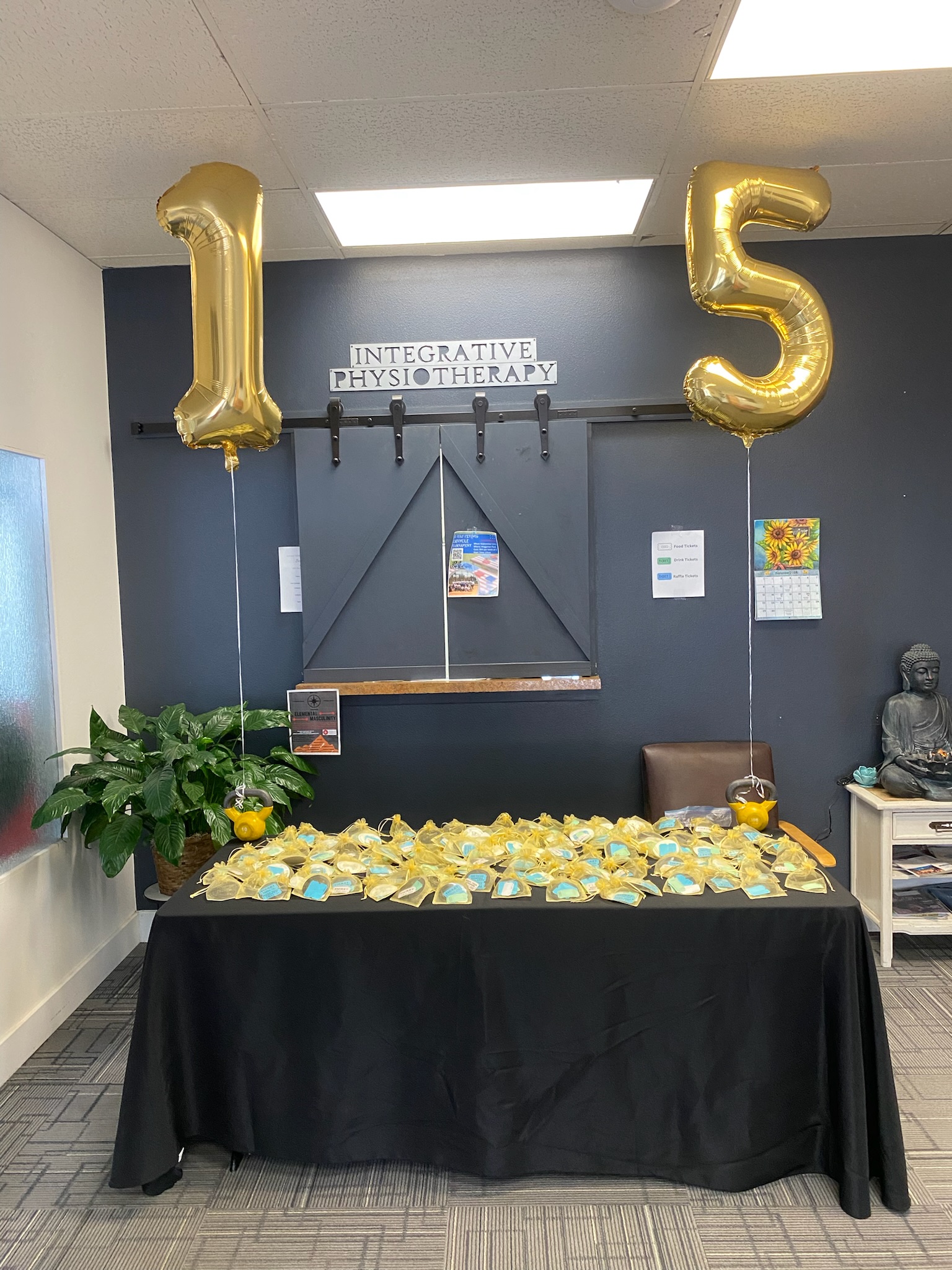
Being ‘healthy’ is more than just avoiding illness or eating fruits and veggies every day. It’s about maintaining balance in your physical, mental and social well-being. While you may begin physical therapy with the goal of reducing pain or healing an injury, PT can also provide significant benefits for your mental health. We recently celebrated 15 years of business. What a milestone! Your team at IP is proud and honored to be apart of the health community in Northern Colorado for over a decade…and we couldn’t have done it without YOU! To show our appreciation, we opened our doors and put our party pants on. There was tacos, yard games, a popcorn machine, IP challenges, prizes and Dr. Ian’s goats!
We recently celebrated 15 years of business. What a milestone! Your team at IP is proud and honored to be apart of the health community in Northern Colorado for over a decade…and we couldn’t have done it without YOU! To show our appreciation, we opened our doors and put our party pants on. There was tacos, yard games, a popcorn machine, IP challenges, prizes and Dr. Ian’s goats!















 So, you’ve decided to trade in your slippers for sneakers, but now you find yourself wondering where to start? How to prevent injuries? How to make it enjoyable? Truth is, all you need is a pair of shoes and a little encouragement to get you out the door.
So, you’ve decided to trade in your slippers for sneakers, but now you find yourself wondering where to start? How to prevent injuries? How to make it enjoyable? Truth is, all you need is a pair of shoes and a little encouragement to get you out the door.

 surgery [surgery is a top one] but PRP, marathon/military training or even activities of daily living are included. Prehab differs from rehab in that it is a proactive plan designed to prepare you for whatever life brings at you next. Here at IP, you know we love pumpin’ prevention to help patients optimize their potential!
surgery [surgery is a top one] but PRP, marathon/military training or even activities of daily living are included. Prehab differs from rehab in that it is a proactive plan designed to prepare you for whatever life brings at you next. Here at IP, you know we love pumpin’ prevention to help patients optimize their potential!
