Run Smarter. Run Stronger.
Jennifer Kummrow2025-04-04T20:56:29+00:00 Running, much like any other skill, takes practice and fine-tuning to improve. Whether you’re lacing up for the first time or you’re a seasoned marathoner, leveling up your performance can be challenging. That’s where a Running Analysis can be a game-changer. Not only can it help increase your performance, it can also help reduce the risk of injury, eliminate pain while running, and optimize your stride!
Running, much like any other skill, takes practice and fine-tuning to improve. Whether you’re lacing up for the first time or you’re a seasoned marathoner, leveling up your performance can be challenging. That’s where a Running Analysis can be a game-changer. Not only can it help increase your performance, it can also help reduce the risk of injury, eliminate pain while running, and optimize your stride!
What is a Running Analysis?
A Running Analysis + Assessment is a two-part approach designed to identify imbalances, weaknesses and areas you may be expending unnecessary energy. Using advanced video technology, we analyze your stride from head to toe, identifying potential issues such as over-striding, knee collapsing, and other imbalances.
So, what are we looking at? The analysis evaluates running mechanics such as:
- Foot strike pattern: How and where your foot makes contact with the ground
- Stride length: The distance covered with each step
- Posture: head/thorax/hip alignment, shoulder symmetry, pelvic tilt, hip position, etc.
- Cadence: The number of steps per minute
What is the Assessment?
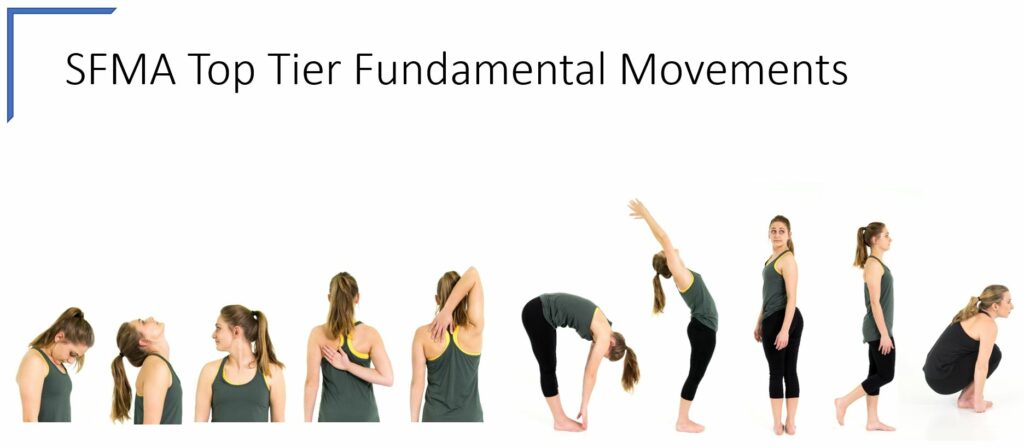
Following the Running Analysis, we conduct the assessment, which goes through a series of tests to examine your strength, stability, and muscle symmetry. We then provide corrective exercises to help balance your strength and enhance your running mechanics.
Is a Running Analysis for me?
The goal of a running analysis is simple: to make you a more efficient, resilient runner. By cleaning up your form, you’ll find yourself feeling good running longer, faster, and stronger- all while reducing your risk of injury!
Your running form is unique to your body. What works for one runner may lead to injury for another. An personalized running analysis ensures that your technique is tailored to your body’s biomechanics, helping you reach optimal performance. By working with our IP therapist/Run Coach, you’ll receive tailored, evidence-based functional tools to mind your movement and a team to support you as you stride!
 The heat gets your heart pumping faster and helps your blood flow better, making it easier for your body to carry oxygen to your muscles. Some people even notice their blood pressure gets lower after using a sauna regularly.
The heat gets your heart pumping faster and helps your blood flow better, making it easier for your body to carry oxygen to your muscles. Some people even notice their blood pressure gets lower after using a sauna regularly. With the new year approaching, many of us are setting goals for personal and professional growth. While working to achieve these goals, it’s important that we remember to prioritize the our bodies, the machines that keep our lives running! Physical therapy can play an essential role in strengthening our resolutions for a healthier, active lifestyle. This new year, let’s not let our injuries limit us from achieving our health and wellness goals. Check out some ways that physical therapy can be beneficial for you when working to become your healthiest ‘elf’!
With the new year approaching, many of us are setting goals for personal and professional growth. While working to achieve these goals, it’s important that we remember to prioritize the our bodies, the machines that keep our lives running! Physical therapy can play an essential role in strengthening our resolutions for a healthier, active lifestyle. This new year, let’s not let our injuries limit us from achieving our health and wellness goals. Check out some ways that physical therapy can be beneficial for you when working to become your healthiest ‘elf’! Here at IP, dry needling is a frequently utilized treatment that contributes to a comprehensive, personalized treatment plan. There are some great benefits to dry needling that include, but are not limited to, quick pain relief, improving range of motion, achieving a quicker path to recovery and more! Dry needling is also called trigger point dry needling or myofascial trigger point dry needling. The word “myofascial” is made up of the roots “
Here at IP, dry needling is a frequently utilized treatment that contributes to a comprehensive, personalized treatment plan. There are some great benefits to dry needling that include, but are not limited to, quick pain relief, improving range of motion, achieving a quicker path to recovery and more! Dry needling is also called trigger point dry needling or myofascial trigger point dry needling. The word “myofascial” is made up of the roots “

 surgery [surgery is a top one] but PRP, marathon/military training or even activities of daily living are included. Prehab differs from rehab in that it is a proactive plan designed to prepare you for whatever life brings at you next. Here at IP, you know we love pumpin’ prevention to help patients optimize their potential!
surgery [surgery is a top one] but PRP, marathon/military training or even activities of daily living are included. Prehab differs from rehab in that it is a proactive plan designed to prepare you for whatever life brings at you next. Here at IP, you know we love pumpin’ prevention to help patients optimize their potential! Exercise of the Month – Bear Crawl [into hibernation]
Exercise of the Month – Bear Crawl [into hibernation] What is Osteoarthritis?
What is Osteoarthritis? 
 As you might have seen in recent social media posts, we’re offering a
As you might have seen in recent social media posts, we’re offering a